CULTURE-PROVEN INFECTIONS IN LATE PRETERM INFANTS IN A NEONATAL INFECTION SURVEILLANCE NETWORK (NEONIN)
C. Kortsalioudaki, I. Kopsidas, E. kourkouni, N. Spyridis, T. Zaoutis, P. Heath
36th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2018)
Malmö, Sweeden, May 28- June 2, 2018
BACKGROUND: Neonatal sepsis is a major cause of neonatal morbidity and mortality especially for the hospitalised neonate. Late preterm (LP) neonates may have a different epidemiology of infections as compared with term neonates, and be at higher risk of infections due to their more immature immune system and the need for NNU-admission after birth. Little data about the risks and epidemiology of infection in LP are published. This study compares the demographics and pathogens responsible for sepsis in the LP infant through the neonIN surveillance network.
METHODS: neonIN is an international web-based surveillance database for culture-proven neonatal infections. Cases of neonates with culture-proven sepsis from participating neonatal-units were extracted and analysed. Late-preterm neonates were defined as those with a gestational age of 33+0 to 36+6 weeks. Repeated growth of the same organism was considered the same episode if occurring within 7 days, or 10 days for Coagulase-negative staphylococci(CONS) and fungi.
RESULTS: 507 LP neonates with culture-proven sepsis were identified. Median birth-weight and a median gestational-age was of 2180g(IQR: 1750-2560) and 34 weeks(IQR:34-36) respectively. Median postnatal-age at the time of infection was 11 days(IQR:3-26). Overall CoNS was the most common pathogen accounting for 40.2%(202) of all cases. When CoNS was excluded the most common pathogen was E. coli(55,10.9%) followed by Klebsiella sp(40,8%),GBS(32,6.4%) and Enterococcus sp(38,7.6%). Characteristics of all cases as well as pathogen distribution by country are displayed on the table below.
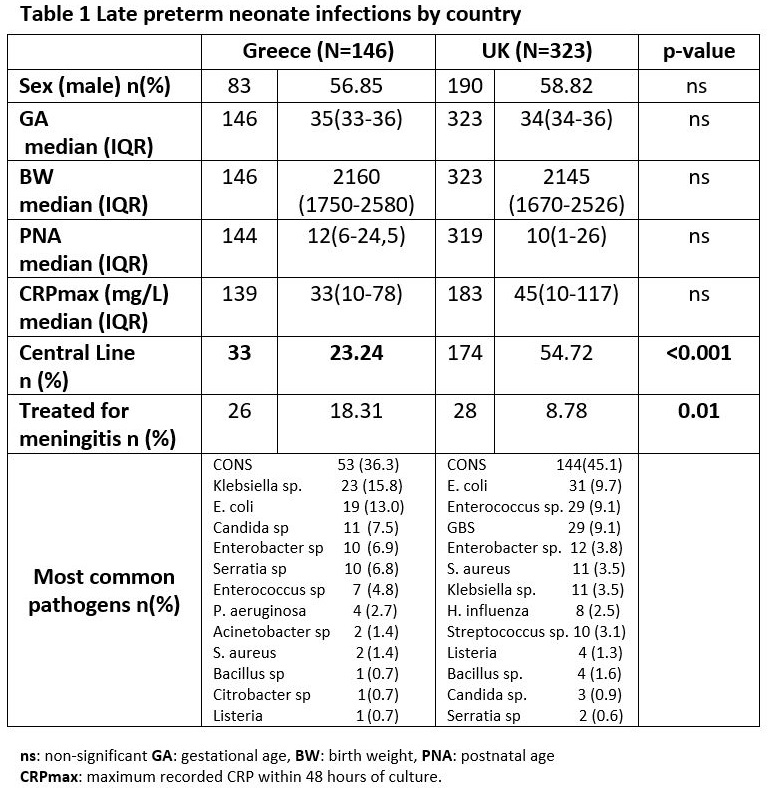
CONCLUSIONS: LP neonates are vulnerable to infection. The closed setting of the neonatal intensive-care and the immunologic immaturity of LP infants make them susceptible to nosocomial infections and they appear to have a distribution of pathogens similar to that of more preterm infants rather than that of term infants



