Key Determinants for the Development of Recurrent Invasive Infections in Neonates: Data from the Neonin Network on Behalf of the Neonatal Infection Surveillance Network (NEONIN)
J. Kopsidas, C. Kortsalioudaki, E. Kourkouni, A. Witney, T. Watts, T. Scorrer, T. Zaoutis, N. Spyridis, P. Heath
35th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2017)
Madrid, Spain, May 23-27, 2017
BACKGROUND: Infection is a major concern in the care of newborn babies. Neonatal infections constitute a major cause of hospital admission and prolonged stay. Recurrent infections contribute to increased mortality and morbidity. This study aims to identify the risk factors associated with recurrent invasive infections in neonates.
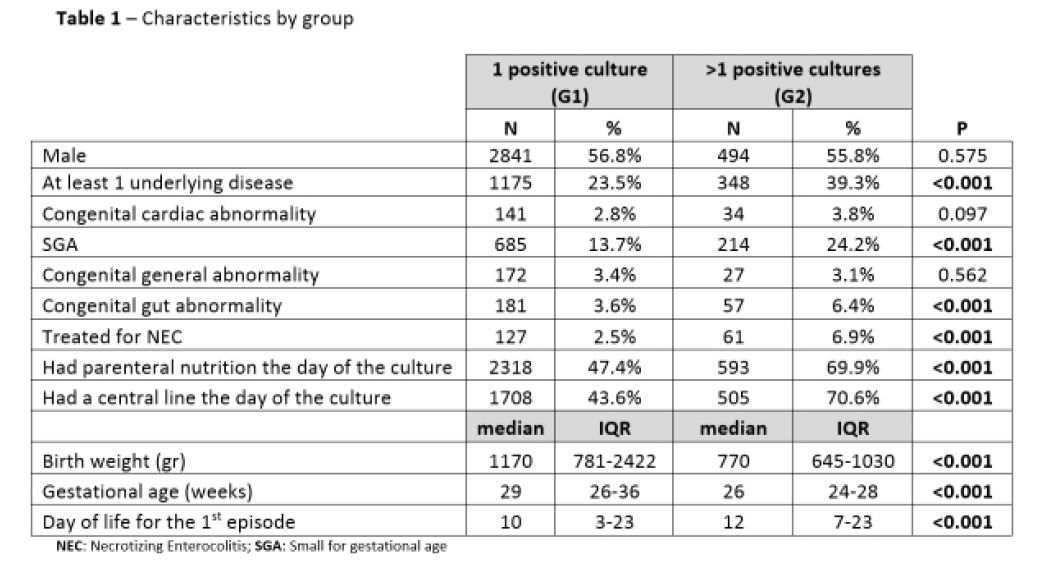
METHODS: neonIN is an international web-based surveillance database for culture proven neonatal infections. Cases from January 2004 to December 2016 were extracted. Two groups were compared: neonates with a single-positive culture (G1) to neonates with recurrentpositive cultures (G2). Repeated cultures with Coagulase-negative staphylococci (CONS) and fungi within 10 days were considered as single episode; for all other pathogens this was limited to 7 days. Associations between the two groups and their characteristics were evaluated with chi-square test of independence and Mann-Whitney test.
RESULTS: We identified 5895 infants, of which 885(15%) with recurrent positive cultures. Neonates with a single-positive culture(G1) had a higher median birth-weight (p<0.001), a higher median gestational-age (p<0.001), were less likely to have received parenteral-nutrition (p<0.001) and to have a central-line present on the day of the culture (p<0.001) compared to the recurrent group (G2). The median day of life for the 1st episode was 10 days(IQR:3-23) vs 12 days(IQR:7-23) (p<0.001) for G1 and G2 respectively. G2 neonates were more likely to have at least one underlying disease 39.3% vs 23.5% (p<0.001). Specifically, they were more likely to be SGA, have congenital gut abnormalities, and been treated for NEC compared to G1. (Table 1) The most commonly isolated pathogen for both groups were CONS (including S.capitis, haemolyticus, warneri and hominis) at 53.3% for G1 vs 59.1% for G2.
CONCLUSIONS: Prematurity, LBW, SGA and GI pathology are important predisposing factors for the development of recurrent bacterial infections.



