Epidemiology of Enterococcus spp. Infections from the Neonin Infection Surveillance Network
J. Wang, C. Kortsalioudaki, P.T. Heath, J. Buttery, T. Watts, T. Scorrer, N. Spyridis, T. Zaoutis, J. Kopsidas, M. Anthony, K. Tan
35th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2017)
Madrid, Spain, May 23-27, 2017
BACKGROUND: Enterococcus spp. cause significant morbidity in neonates, particularly critically-ill neonates hospitalised in the NICU. This study describes the epidemiology of neonatal enterococcal infections across a network of NICUs, with the aim of informing infection prevention strategies.
METHODS: neonIN is a multi-national neonatal infection surveillance network which records prospectively-collected infection data from 60 units in the UK, Greece, Estonia and Australia. All infection cases reported to neonIN from 2004 to May 2016 were extracted. Infection was defined as a positive culture from a sterile site (e.g. blood, cerebrospinal fluid). Early and late-onset infection were defined as infection before or after 48 hours of life respectively. Statistical analyses (including multivariate regression) were performed using the Stata 14 statistical package.
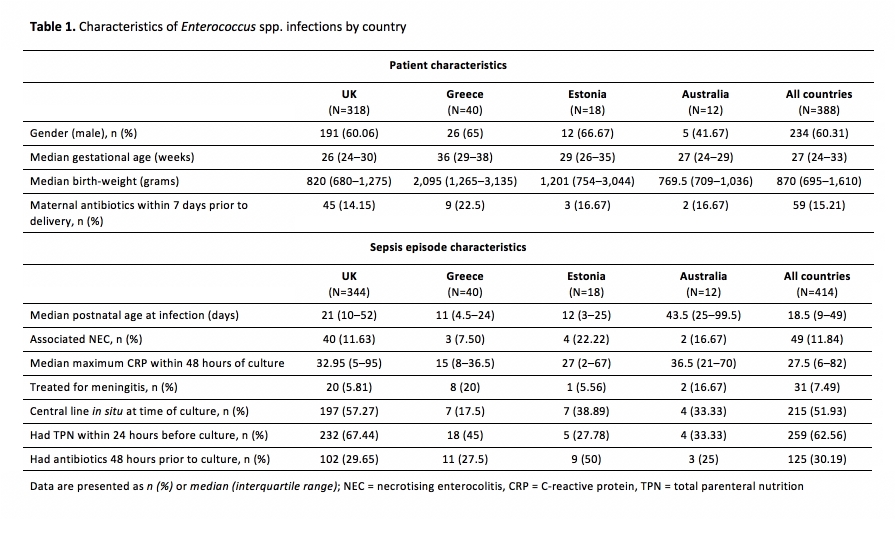
RESULTS: 414 enterococcal infections were reported in 388 infants (total of 4,083 infection episodes in 3,602 infants). Enterococci were the 2nd most common cause of late-onset infection (385/3,481 isolates). Table 1 presents enterococcal infection characteristics by country. On multivariate analysis, compared to other infections, enterococcal infections occurred at a greater median postnatal age (18.5 versus 13 days, p<0.001), and were strongly associated with NEC (OR 1.50, 95%CI 1.08-2.10, p=0.017). Antimicrobial susceptibilities were available for 288/416 (69%) enterococcal isolates. There was low resistance to vancomycin (3%) and teicoplanin (4%), but high resistance to ampicillin (17%) and gentamicin (38%).
CONCLUSIONS: We demonstrated an association between neonatal enterococcal infection and NEC, suggesting that NEC prevention may also have a role in reducing these infections. Further, enterococci were frequently resistant to first line empirical antibiotics such as ampicillin and gentamicin – of relevance in considering empiric antimicrobial policies.



