HOSPITAL-ACQUIRED INFECTION SURVEILLANCE AMONG 11 EUROPEAN COUNTRIES. A RANIN-KIDS SURVEY
I. Kopsidas, J. Bielicki, D. Blázquez-Gamero, A. Brett, M. Collins, R. Cunney, M. De Luca, D. Dona, S. Drysdale, C. Epalza, O. Falup-Pecurariu, E. Iosifidis, N. Klein, I. Lutsar, A. Mougkou, O. Neth, W.G. Valdivia, J. Saavedra, M. Tsolia, U. von Both, S. Vergnano, S. Patel, T. Zaoutis, N. Spyridis.
37th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2019)
Ljubljana, Slovenia, 6-11 May, 2019
BACKGROUND: RANIN-KIDS (Reducing Antimicrobial use and Nosocomial INfections in KIDS) is a collaborative European effort that aims to create a unified surveillance mechanism for pediatric HAIs and antibiotic use in Europe and to implement interventions to prevent HAIs and to promote antimicrobial stewardship (ASP). In December 2018, an electronic survey that included questions on HAI surveillance and prevention practices was created and disseminated among members of the RANIN network.
METHODS: A two phase (pre- and post-intervention) active surveillance mechanism for HH was established in 15 NICUs throughout the country. Observations were conducted from June 2016 to June 2018 using a data collection tool based on WHO guidelines. Compliance rate was defined as [(number of performed actions)/(number of opportunities)]x100. An intervention that included HH training as part of a care bundle for central line-associated bloodstream infections was implemented from March to April 2017 and consisted of on-site staff training, educational material, and reminders in the workplace such as posters, brochures and rulers representing ‘’The Five Moments of HH’’ and appropriate hand-washing technique.
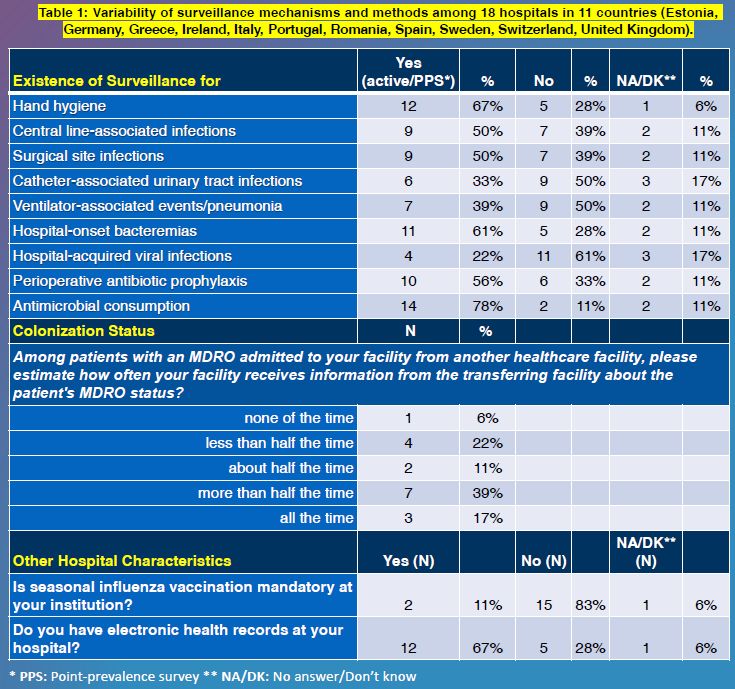
RESULTS: 18 teaching hospitals from 11 countries submitted data. All but two reported having formal infectious diseases (ID) teams. Only 1 reported having no infection control (IC) team. Surveillance programs for HAIs were reported as follows: CLABSI 50%, CAUTI 33%, and VAP 39%. Only 22% reported having surveillance programs for hospital-acquired viral infections (Table 1). Hand hygiene practices were monitored by 67% of hospitals. In almost 40% of hospitals, information related to multidrug-resistant organisms carriage is unavailable in at least half of transferring patients.
CONCLUSIONS: Preliminary results on HAI surveillance practices showed that while the majority of hospitals surveyed have ID teams and IC nurses, surveillance of HAIs is significantly lacking. The results of this survey will be used to inform the creation of a unified surveillance mechanism for pediatric HAIs in Europe and to design preventative interventions.