Greek medical students’ perceptions, knowledge, and education about antimicrobial prescribing and resistance: a cross-sectional study
I. Kopsidas , G. Kurtzman , M. Mitrou , G.C. Tsopela , G. Papantoniou , E. Agathocleous , F. Alexiou , M. Belevegka , M.I. Karatza , M. Konstantinis , S. Prapiadou , C. Triantafyllou , N.M. Molocha , E. Kourkouni , T. Zaoutis
37th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2019)
Ljubljana, Slovenia, 6-11 May, 2019
BACKGROUND: Injudicious use of antibiotics is a major cause of antimicrobial resistance, which increases morbidity, mortality and health-care costs. WHO has highlighted the importance of undergraduate training in prudent antibiotic use. In Greece, a country burdened with high antibiotic consumption and resistance, little is known about students’ knowledge on antibiotic prescribing. We aimed to assess Greek medical students’ perceptions, knowledge, and education about antimicrobial prescribing and resistance(AMPR).
METHODS: Α voluntary, anonymous, cross-sectional survey of final-year medical students was conducted in 6/7 medical schools in Greece, consisting of 40 questions on perceptions, knowledge, and education about AMPR. The survey was disseminated by HelMSIC (Hellenic Medical Students’ International Committee) between 26/11/2018 and 7/12/2018.
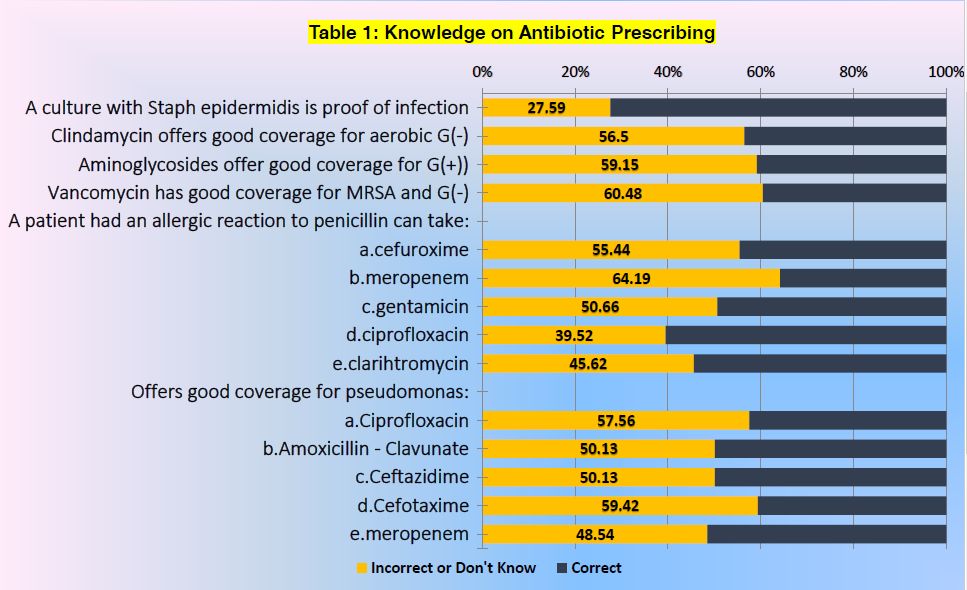
RESULTS: The survey had a response rate of 60.3% (375/622). 71.5% had never heard the term Antibiotic Stewardship. 55% answered correctly to half or fewer of 14 questions on antibiotic prescribing (Table1). The majority failed to identify that vancomycin (59%) and clindamycin (57.8%) do not have good coverage for gram-negative bacteria. Students could not identify as inappropriate antimicrobials for an ESBL infection: amphotericin-B (84.3%), vancomycin (85.1%), linezolid (93.4%), or ceftriaxone (40%).Only 16% would prescribe amoxicillin to a fully immunized thirteen-year-old with community-acquired pneumonia. Throughout medical school respondents had been asked fewer than 5 times or not at all to choose: whether an antibiotic was needed (57.3%); the right antibiotic (48.5%); route, dose, and interval (71.2%); duration (62.3%); or the agent based on the culture results (67.4%). Self-reported confidence on 15 items regarding antimicrobial prescribing (on a scale from 1[not at all] to 10[totally]) was a mean of 6.28/10.
CONCLUSIONS: We identified considerable gaps in knowledge of AMPR and inadequate practical training among Greek medical students, which impacts their confidence in these areas.These targets will educate the design of an intervention that could tackle Greece’s problem of injudicious antimicrobial use and resistance at its root: the medical school.